 The horny layer of the skin is able both to prevent the loss of fluid and electrolytes, and to stop the penetration of harmful substances. It is a dry mechanical barrier from which contaminating organisms and chemicals are continually being removed by washing and desquamation. Only when these breach the horny layer do the cellular components, described below, come into play. The skin is involved in so many immunological reactions, seen regularly in the clinic.. More diseases are now being classified by abnormalities of function and structure rather than by their appearance.Today’s patients are inquisitive and knowledgeable. If you understand the structure and function of the skin, your explanations to them will be easier and more convincing.
The horny layer of the skin is able both to prevent the loss of fluid and electrolytes, and to stop the penetration of harmful substances. It is a dry mechanical barrier from which contaminating organisms and chemicals are continually being removed by washing and desquamation. Only when these breach the horny layer do the cellular components, described below, come into play. The skin is involved in so many immunological reactions, seen regularly in the clinic.. More diseases are now being classified by abnormalities of function and structure rather than by their appearance.Today’s patients are inquisitive and knowledgeable. If you understand the structure and function of the skin, your explanations to them will be easier and more convincing.
that a special mention has to be made of the peripheral arm of the immune system based in the skinathe skin immune system (SIS). The idea of an SIS as a functionally independent immunological unit is helpful. It includes the cuta neous blood vessels and lymphatics with their local lymph nodes and contains circulating lymphocytes and resident immune cells. Although it is beyond the scope of this book to cover general immunology, this section outlines some of the intricate ways in which antigens are recognized by specialized skin cells, mainly the Langerhans cells, and how antibodies, lymphocytes, macrophages and polymorphs elicit inflammation.
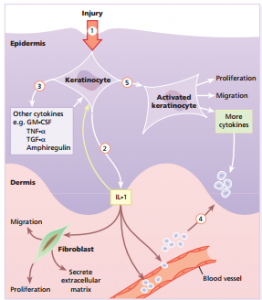
Some cellular components of the skin immune system Keratinocytes Their prime role is to make the protective horny layer and to support to the outermost epithelium of the body but they also have immunological functions in their own right. Keratinocytes produce large numbers of cytokines , and can be induced by γ-interferon to express HLA-DR. They can also produce α-melanocyte-stimulating hormone which is immunosuppressive. Keratinocytes play a central part in healing after epidermal injury . Langerhans cells These dendritic cells come from the bone marrow and circulate through the epidermis, the dermis, lymphatics (as ‘veiled cells’), and also through the T-cell area of the lymph nodes where they are called ‘dendritic’ or ‘interdigitating’ cells. They can be identified in tissue sections by demonstrating their characteristic surface markers (e.g. CD1a antigen, MHC Class II antigens, adenosine triphosphatase) or S-100 protein in their cytoplasm (also found in melanocytes). Langerhans cells have a key role in antigen presentation. Dermal dendritic cells These poorly characterized cells are found around the tiny blood vessels of the papillary dermis. They bear MHC Class II antigens on their surface and,




